Table of Contents

The birth of a newborn is the purest moment of joy, but babies may face a few common health concerns, with one of the most common ones being jaundice in newborns. It is a mild condition that causes the baby to develop a yellowish tint on the skin and eyes, and is common in most babies in India and globally. The promising news? It is usually short-term and is manageable through soft treatment of newborn jaundice and observation.
Neonatal jaundice is a condition in which the skin and the whites of the eyes of a newborn assume a yellow appearance because of increased bilirubin in the blood. Bilirubin is a natural substance formed when red blood cells break down. Newborns have not yet fully developed their liver, which is involved in the breakdown of bilirubin, so there is a temporary effect of increasing levels of bilirubin.
There are different types of newborn jaundice, including:
Babies often develop jaundice because their bilirubin levels are higher, and their livers need time to adjust with bilirubin. In India, studies suggest that over half of full-term newborns may experience jaundice in their first week within the initial week of life. Neonatal jaundice is quite common in newborn babies. In India, studies show that it affects between 60% and 80% of newborns.
In the majority of circumstances, neonatal jaundice is minimal and self-limiting. However, a medical assessment is vital to ensure that the level of bilirubin stays within a safe limit.
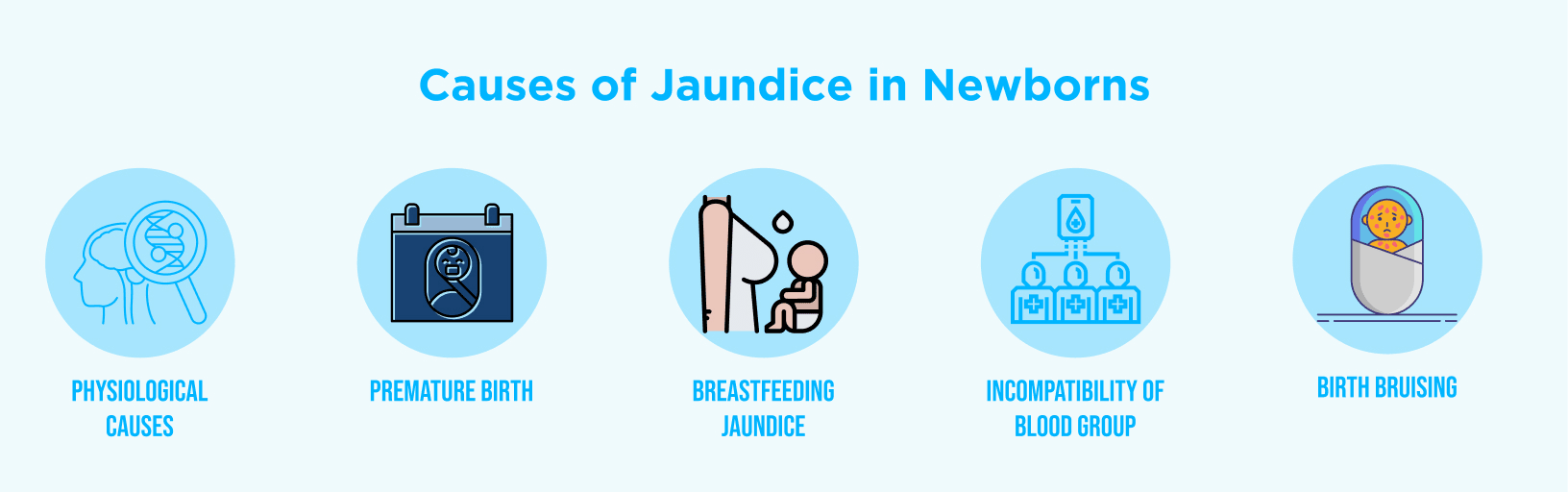
Here are some causes of jaundice in newborn:
The symptoms of jaundice in newborns are not difficult to notice:
When you see these symptoms of newborn jaundice, visit a paediatrician immediately. Choosing the right child specialist early on helps parents feel confident about managing newborn health concerns. To get the best possible neonatal jaundice therapists, visit the best paediatrician for newborn care.
It is necessary to diagnose jaundice in newborns early to prevent the development of complications. During birth and the initial days, the doctors pay close attention to the yellow color of your baby’s skin, gums, and eyes. Diagnosis may involve:
Newborn jaundice treatment offers newborn screening that can identify jaundice before it becomes a serious condition, so the level of slight jaundice in newborn can be corrected early, and parents will be relieved that their baby is doing fine.
According to a study conducted at SMS Medical College in Jaipur, about 60% of full-term newborns and up to 80% of preterm babies develop neonatal jaundice in their first week of life.
Newborn jaundice is treated based on the level of bilirubin, age of the infant, and cause of jaundice:
Newborns receive round-the-clock observation and personalised care plans to ensure safe, gentle, and effective recovery.
Yes, breastfeeding jaundice may occur in the first few days if the baby receives less milk, which can slow bilirubin removal.However, the process of breastfeeding aids in recovery as well; the more the baby is fed, the more water he will get, and the faster the bilirubin will be eliminated. Most times, you are advised to keep breastfeeding, and this will be under the supervision of your paediatrician.
Jaundice in newborns can seem worrying to parents, but it is usually temporary and manageable.. Most babies can recover within a short time with timely diagnosis, gentle monitoring and effective treatment options such as phototherapy, hence they continue to thrive. The most important thing is a timely response and constant monitoring by skilled medical treatment specialists. Alongside newborn care, staying updated with essential immunizations ensures that babies remain protected against preventable diseases.
Our team at Best Super Multispeciality Hospital in Chennai brings a distinct mixture of competence and caring to help parents through all the steps of the procedure, so your baby is provided with the safest and best beginning in life. As a team, we guide your baby through the jaundice recovery time newborn process to a healthy glow with confidence.
Table of Contents
Recent Post
About us
Dr. Mehta’s Hospitals is a leading multispecialty hospital in Chennai with over 90 years of excellence. With 400+ beds and 80+ specialties, its Chetpet and Velappanchavadi centers offer advanced, state-of-the-art, compassionate care under one roof.
Chetpet Contact Details
Velappanchavadi Contact Details
Feel free to ask your queries on
Our Specialities
About us
Dr. Mehta’s Hospitals is a leading multispecialty hospital in Chennai with over 90 years of excellence. With 400+ beds and 80+ specialties, its Chetpet and Velappanchavadi centers offer advanced, state-of-the-art, compassionate care under one roof.
Chetpet Contact Details
Velappanchavadi Contact Details
Feel free to ask your queries on
Our Specialities
Quick Links
Center of excellence