What is Uterine Fibroids?
Uterine fibroids are a common type of noncancerous tumor that can grow in and on your uterus. Not all fibroids cause symptoms, but when they do, symptoms can include heavy menstrual bleeding, back pain, frequent urination and pain during sex. Small fibroids often don’t need treatment, but larger fibroids can be treated with medications or surgery.
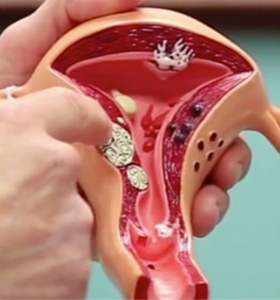
Uterine fibroids (also called leiomyomas) are growths made up of the muscle and connective tissue from the wall of the uterus. These growths are usually not cancerous (benign). Your uterus is an upside down pear-shaped organ in your pelvis. The normal size of your uterus is similar to a lemon. It’s also called the womb and it’s the place where a baby grows and develops during pregnancy.
Fibroids can grows as a single nodule (one growth) or in a cluster. Fibroid clusters can range in size from 1 mm to more than 20 cm (8 inches) in diameter or even larger. For comparison, they can get as large as the size of a watermelon. These growths can develop within the wall of the uterus, inside the main cavity of the organ or even on the outer surface. Fibroids can vary in size, number and location within and on your uterus.
You may experience a variety of symptoms with uterine fibroids and these may not be the same symptoms that another woman with fibroids will experience. Because of how unique fibroids can be, your treatment plan will depend on your individual case.
Symptoms of Uterine Fibroids
Many women who have fibroids don’t have any symptoms. In those that do, symptoms can be influenced by the location, size and number of fibroids.
In women who have symptoms, the most common signs and symptoms of uterine fibroids include:
- Heavy menstrual bleeding
- Menstrual periods lasting more than a week
- Pelvic pressure or pain
- Frequent urination
- Difficulty emptying the bladder
- Constipation
- Backache or leg pains
Rarely, a fibroid can cause acute pain when it outgrows its blood supply, and begins to die.
Fibroids are generally classified by their location. Intramural fibroids grow within the muscular uterine wall. Submucosal fibroids bulge into the uterine cavity. Subserosal fibroids project to the outside of the uterus.
Causes of Uterine Fibroids
Doctors don’t know the cause of uterine fibroids, but research and clinical experience point to these factors:
Genetic changes. Many fibroids contain changes in genes that differ from those in normal uterine muscle cells.
Hormones. Estrogen and progesterone, two hormones that stimulate development of the uterine lining during each menstrual cycle in preparation for pregnancy, appear to promote the growth of fibroids.
Fibroids contain more estrogen and progesterone receptors than normal uterine muscle cells do. Fibroids tend to shrink after menopause due to a decrease in hormone production.
Other growth factors. Substances that help the body maintain tissues, such as insulin-like growth factor, may affect fibroid growth.
Extracellular matrix (ECM). ECM is the material that makes cells stick together, like mortar between bricks. ECM is increased in fibroids and makes them fibrous. ECM also stores growth factors and causes biologic changes in the cells themselves.
Doctors believe that uterine fibroids develop from a stem cell in the smooth muscular tissue of the uterus (myometrium). A single cell divides repeatedly, eventually creating a firm, rubbery mass distinct from nearby tissue.
The growth patterns of uterine fibroids vary — they may grow slowly or rapidly, or they may remain the same size. Some fibroids go through growth spurts, and some may shrink on their own.
Many fibroids that have been present during pregnancy shrink or disappear after pregnancy, as the uterus goes back to a normal size.
When to See Your Doctor
Call your doctor if you have any of the following issues, including:
- Chronic pelvic pain
- Difficulty emptying bladder
- Inability to control urine flow
- Very heavy, painful periods
- Lump or mass in your abdomen
You should see your doctor immediately if you have uncontrollable bleeding, or sudden sharp pelvic pain.