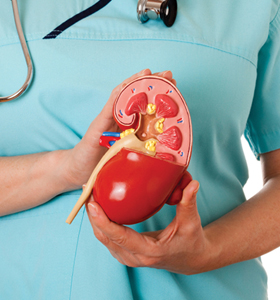
Diabetic kidney disease is a decrease in kidney function that occurs in some people who have diabetes. It means that your kidneys are not doing their job as well as they once did to remove waste products and excess fluid from your body. These wastes can build up in your body and cause damage to other organs.
Cause of diabetes kidney disease
High blood glucose, also called blood sugar, can damage the blood vessels in your kidneys. When the blood vessels are damaged, they don’t work as well. Many people with diabetes also develop high blood pressure, which can also damage your kidneys. Learn more about high blood pressure and kidney disease.
Symptoms of diabetes kidney disease
You are unlikely to have symptoms with early diabetic kidney disease – for example, if you just have microalbuminuria (defined above). Symptoms tend to develop when the kidney disease progresses. The symptoms at first tend to be vague and nonspecific, such as feeling tired, having less energy than usual and just not feeling well. With more severe kidney disease, symptoms that may develop include:
- Difficulty thinking clearly.
- A poor appetite.
- Weight loss.
- Dry, itchy skin.
- Muscle cramps.
- Fluid retention which causes swollen feet and ankles.
- Puffiness around the eyes.
- Needing to pass urine more often than usual.
- Being pale due to anaemia.
- Feeling sick (nausea).
As the kidney function declines, various other problems may develop – for example, anaemia and an imbalance of calcium, phosphate and other chemicals in the bloodstream. These can cause various symptoms, such as tiredness due to anaemia, and bone ‘thinning’ or fractures due to calcium and phosphate imbalance. End-stage kidney failure is eventually fatal unless treated.
Diabetic kidney disease diagnosis
Diabetic kidney disease is diagnosed when the level of albumin in the urine is raised and there is no other obvious cause for this. Urine tests are part of the routine checks that are offered to people with diabetes from time to time. Urine tests can detect albumin (protein) and measure how much is present in the urine.
The standard routine urine test is to compare the amount of albumin with the amount of creatinine in a urine sample. This is called the albumin:creatinine ratio (ACR). Creatinine is a breakdown product of muscle.
A blood test can show how well the kidneys are working. The blood test measures the level of creatinine, which is normally cleared from the blood by the kidneys. If your kidneys are not working properly, the level of creatinine in the blood goes up. An estimate of how well your kidneys are working can be made by taking into account the blood level of creatinine, your age and your sex. This estimate of kidney function is called the estimated glomerular filtration rate (eGFR).